WTA Toolkit for Violence Prevention Programming
WTA Toolkit for Violence Prevention Programming
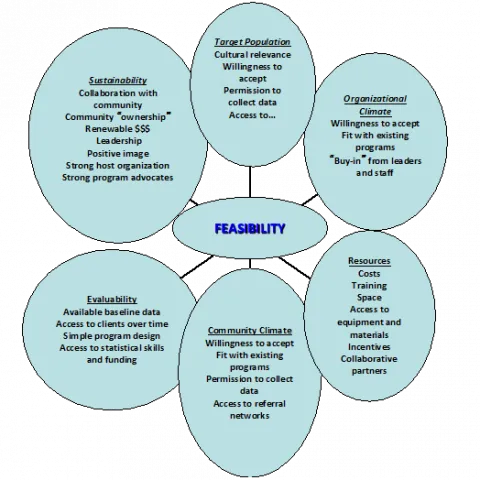
Hospital-based and hospital-linked violence prevention, intervention and interruption programs are being disseminated at a fast pace across the country. Interest in starting programs is accelerating. These programs have different areas of focus, but they all aim to address the epidemic of violence that continues to plague our people. As health care providers caring for the injured, we have a unique opportunity to bring these programs directly to our patients but doing so can be complex. The Feasibility Diagram below illustrates the elements necessary to consider when implementing and sustaining these types of injury prevention programs.
Advocacy is an activity that requires data, cultural humility, creativity, and flexibility. The right message is required for the right stakeholder. The following toolkit is meant to serve as an aid in advocacy when working to implement a violence prevention program at a trauma center. This guide is meant to assist in naming important elements in correspondence with a variety of stakeholders, all of whom have a critical stake in violence prevention. It is meant to aid in the context of the elements listed in the Feasibility Diagram.
- Addressing the communities impacted by violence
Building trust with the communities impacted by violence is an essential principle in starting and maintaining a violence prevention program. For many of our communities, there is deep mistrust in the health care system. We need to acknowledge this and move forward. Whether we intend to have a hospital-based or hospital-linked program, community leaders need to be equal partners in the development of the program. Community representatives are most capable of serving as frontline workers, otherwise known as Violence Prevention Professionals. Establishing partnerships with community organizers/community-based organizations leads to opportunities for creating essential elements such as data sharing agreements and memoranda of understanding. Listed below are essential features in developing this partnership:
- Meet prospective partners outside of the hospital, in the community. This demonstrates commitment and establishes equality.
- Incorporate community leaders in the process of hiring of frontline workers
- When presenting information on the burden of injury, invite the community’s input on the impact it has on The community does not necessarily need us to explain to them the impact of violence
- Do your homework on what else currently exists in the area around violence prevention so as not to exclude key stakeholders. Invite information that you need to learn from the community as to what is happening around violence prevention. Skipping this step has created major pitfalls in programs across the country
- Understand what it means to have cultural humility
- Plan to meet regularly with CBOs. If the program is hospital-linked with the CBO providing the frontline services, this is even more critical. Renewing relationships, checking in (outside of the hospital), and making sure that the community’s ideas are incorporated into programming will maintain program relevance and build trust.
- Know that resources exist for aid in training and technical assistance. thehavi.org is one such place when considering hospital-based or hospital-linked violence intervention programming (HVIPs)
- Addressing local and regional policymakers
Although the COVID-19 pandemic raised significant awareness regarding racial disparities in health, violent injury has always stood as a striking example of the vulnerability of black and brown populations to the impact of social determinants of health. When addressing our policymakers, it is important to have a clear understanding of the local impact of violence, the importance it is to you and to the policymaker and to his/her constituents, and finally your ask. Many HVIPs are funded through city and county mechanisms such at the Department of Public Health, line items in Mayors’ budgets, Departments of Children, Youth and Families and other mechanisms. In addition, taxonomy has been approved in CMS for the position of Violence Prevention Professional (frontline worker). Under this, taxonomy, two states have passed legislation allowing for Violence Prevention Professionals to bill for services rendered, making sustainability of these programs much more promising. A few tips for discussions with Policymakers:
- State the local impact of violent injury on their constituency: Know your data but do not get too technical, unless asked
- Talk about the issue in your own personal experience and strongly consider doing this with one of your partners from the community or with someone directly impacted by violence. Discuss the value of integrating social care into the trauma care system and the essential nature of working with community to achieve this
- Be ready with your ask: What is your proposal? How much will it cost?
- Discuss the progress of sustainability in terms of CMS. Consider mentioning that Illinois and Connecticut have already passed legislation on this. Mention other precedents elsewhere (The HAVI can help with this) and other sources of funding such as Office of Victim of Crime.
- Addressing hospital leadership and trauma center leadership
Community Health Needs Assessments are essential for hospitals to conduct. Under Section 501 (r)(3)(a), a hospital must conduct a CHNA every three years and implement strategies to address the needs (https://www.irs.gov/charities-non-profits/community-health-needs-assessment-for-charitable-hospital-organizations-section-501r3) . In addition, Level I and II trauma centers must implement programs that address a major cause of injury in the community (CD 18-5) per the Resources for the Care of the Injured Patient (https://www.facs.org/-/media/files/quality-programs/trauma/vrc-resources/resources-for-optimal-care.ashx ). These guidelines provide a foundation by which we can advocate for violence intervention programming as a way of addressing the requirements with our hospital leadership and trauma program leadership.
- Similar to policymakers, go to hospital leadership with the issue, the impact, and the solution
- Discuss the inherent value of working with the hospital’s surrounding community to address violent injury together
- Offer suggestions regarding notoriety through media of implementing and growing a program that directly affects the community at large
- Discuss the value of having a program in violence prevention in the portfolio of the hospital’s foundation/development office
- The COT has recently invested significant effort into advocacy and development of best practices in HVIP work. Providing this broader context can also be a powerful talking point in advocacy. See recent COT references below.
- J Am Coll Surg. 2019 Oct;229(4):415-430.e12. doi: 10.1016/j.jamcollsurg.2019.05.018. Epub 2019 May 17. PMID: 31108194
- J Am Coll Surg. 2021 Sep;233(3):471-478.e1. doi: 10.1016/j.jamcollsurg.2021.06.016. Epub 2021 July 30. PMID: 34446220
- Addressing departmental, academic leadership
Social determinants of health are responsible for approximately 40% of our overall state of wellness. Incorporation of social constructs into medical school curricula is happening rapidly across the country as awareness is raised. Along with the education component, research and evaluation in public health, population health, translational social science and implementation science is becoming more commonplace as recognition of its importance in improving care of our injured and sick patients is more appreciated. Research tracks at major Universities and clinical departments now exist in the field of public health and population health
- There is tremendous opportunity for scholars to be involved in research and evaluation in violent injury epidemiology and both qualitative and quantitative analysis of violence prevention programming
- There is a Firearm Prevention Research Scholar (a resident in research years) selected through a combined effort of the AAST, COT, WTA, PSA, EAST.
- NIH and CDC has increased funding in the field of violence prevention significantly over the past two years
- Career development can be supported by a growing number of research scholars in this area
Violence Intervention development, implementation and sustainability is predicated on building an array of relationships. Investment from a multitude of stakeholders is necessary for success. We hope that this toolkit provides a useful framework by which you can feel empowered to go out and make it happen in your trauma center.